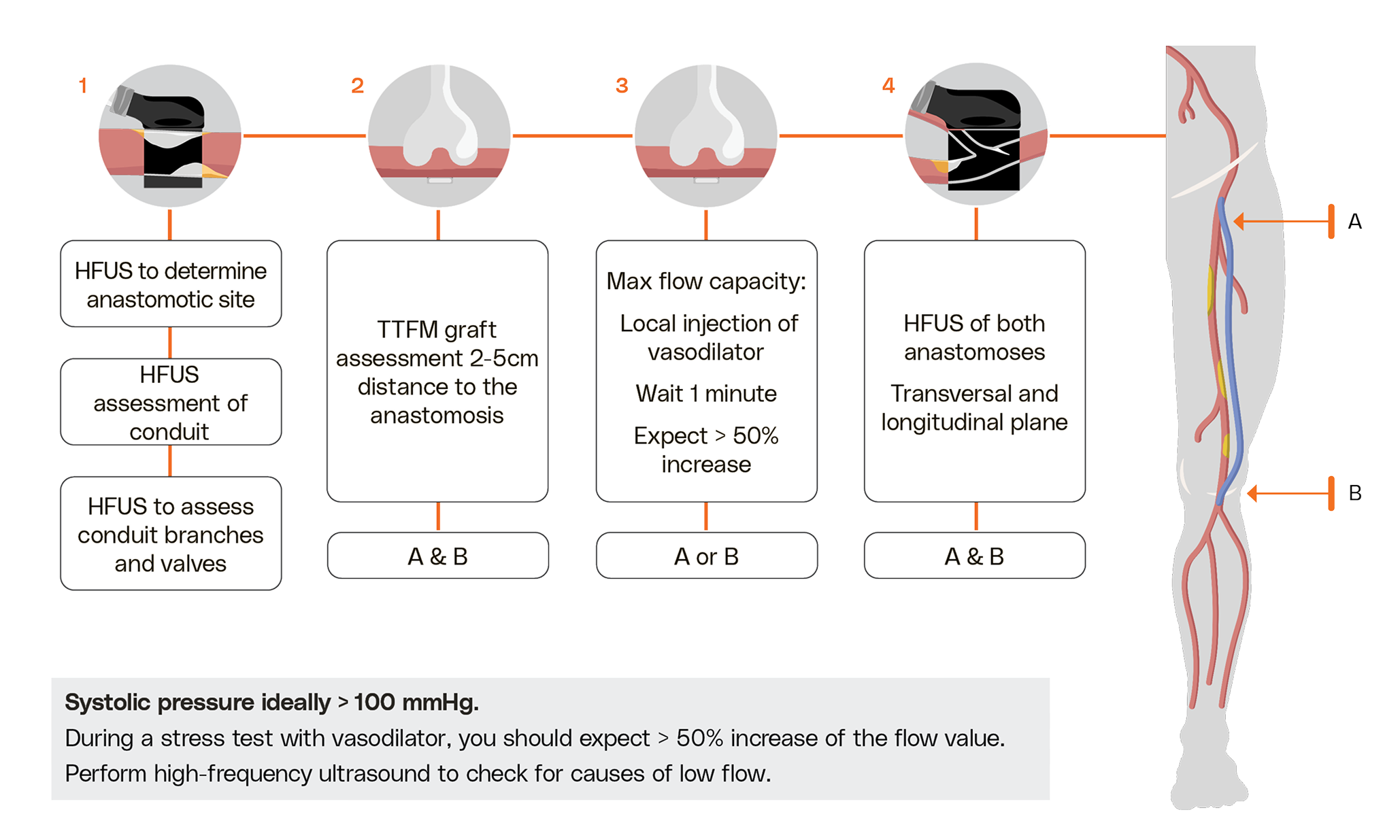
Peripheral Bypass
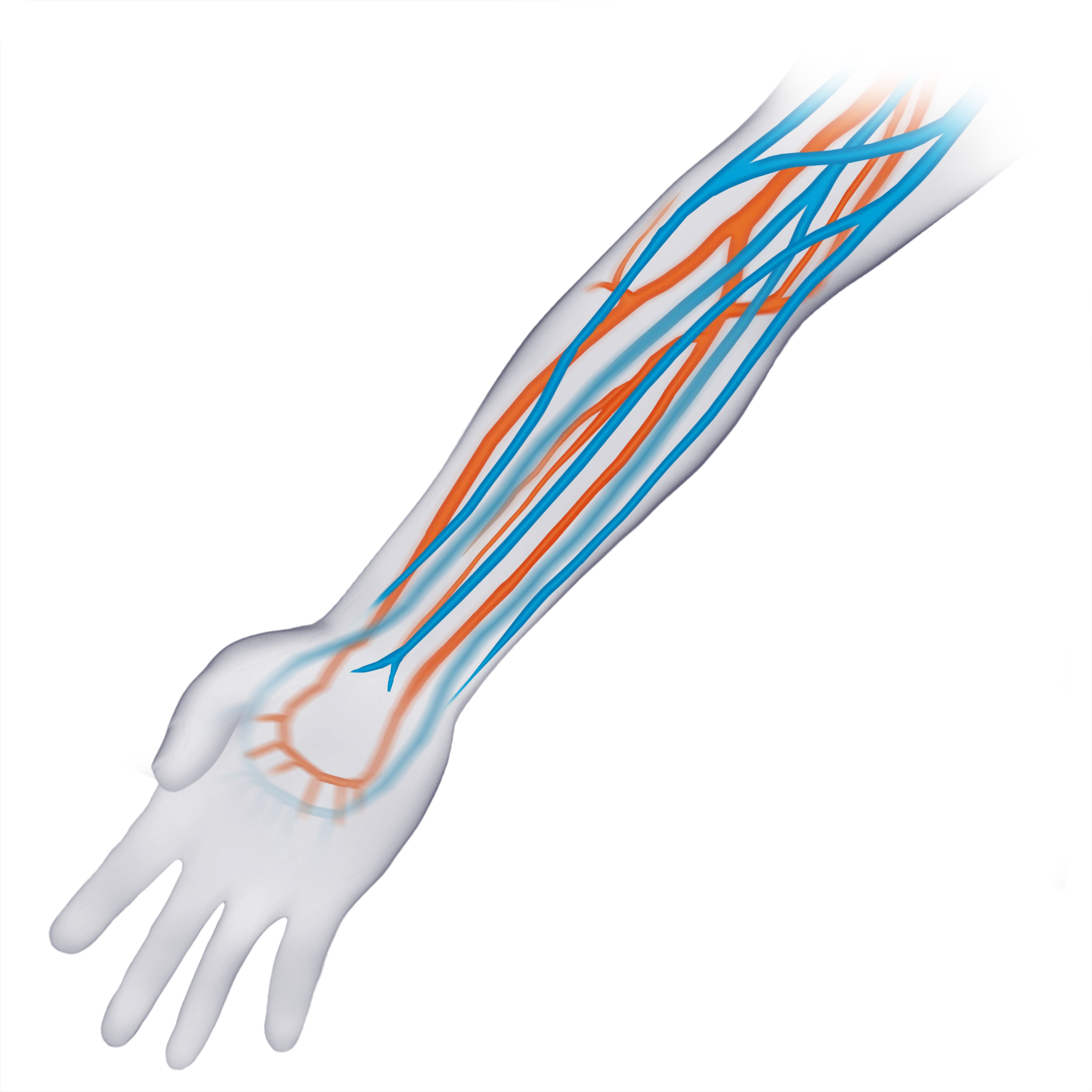
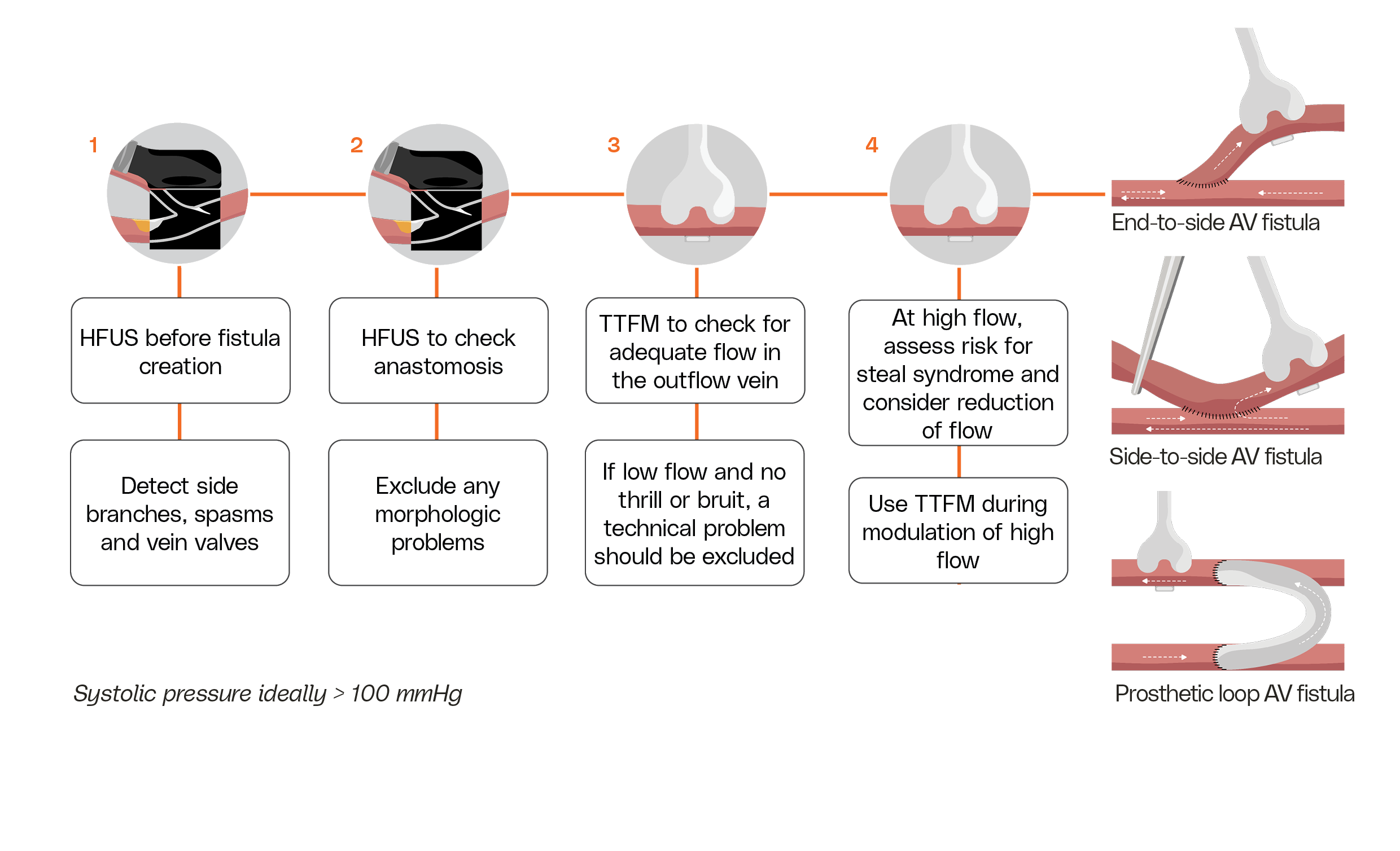
Critical limb-threatening ischemia (CLTI) is the most advanced stage of peripheral artery disease and greatly increases the risk of limb loss. Medistim provides an intraoperative quality assessment system that combines flow measurement and imaging to give immediate feedback on graft patency and enable revision before closure. Volumetric flow values are key for predicting graft longevity, and low flow or lack of response to a vasodilator stress test indicates higher risk of early occlusion. Medistim’s imaging probe can reveal hidden anastomotic imperfections, allowing surgeons to correct issues during surgery. Because graft patency strongly predicts long-term outcomes, this technology helps improve patient survival and limb salvage.